1.0 INTRODUCTION
Nigeria has a reputation for being a very
violent country. In 2014, it was considered to be the seventeenth most fragile
state in the world, and it was ranked 151 out of 162 countries in the Global
Peace Index, a multidimensional report on violence, security, and criminality
(Marc- Antonies, 2014). Literature on causes of violence in Nigeria identifies many factors among them selfishness,
greed, injustice, do-or-die politics, love of money, wealth, accumulation of
wealth, revolt, repression, immorality, and ignorance, etc. Violence in
Nigeria in its various forms has evolved over the decades; from the use of
traditional weapons, charms, and hamlets, violence in Nigeria has taken a sophisticated dimension. Political, electoral, religious, ethnic/tribal, cultism, and other forms of violence are dominant in Nigerian society, at varying
degrees. Each region in Nigeria has its peculiar form of violence; in northern
Nigeria, religious violence and extremist attacks are peculiar, in the
South-South, militancy is popular and like extremist attacks in northern
Nigeria, it has received global attention. In the Southeast, cultism ferocity, and robbery attacks are common forms of violence, while in the Southwest,
political violence and thuggery are intrinsic. However, this doesn’t mean other
forms of violence such as gender-based violence (rape, abuse, intimidation), and tribal clashes among others still exist across the regions of Nigeria (Rotimi,
2019).
2.0 DISCUSSION
Accordance to the World Health Organization’s Violence Prevention Alliance1,
‘violence’ is the intentional use of physical force or power, threatened or actual,
against oneself, another person, or against a group or community, that either
result in or has a high likelihood of resulting in injury, death,
psychological harm, maldevelopment, or deprivation. This includes neglect,
physical, sexual, and psychological violence, and can be interpersonal (towards
a family member, partner, acquaintance, or stranger), self-directed, or
committed by larger groups such as nation-states and terrorist organizations (WHO 2017c).
Addressing violence is not a
single-agency issue, as it is the culmination of many different issues. It is
only by pursuing a strategic, coordinated approach involving a range of
agencies, including partnerships between statutory and voluntary organizations,
that violent crime can be effectively addressed. Therefore, it is imperative to
look into the topic of the public health approach to violence prevention in Nigeria.
The World Health Organization (WHO)
(2017a) defines a public health approach to reducing violence as one that: ‘Seeks to improve the health and safety of all
individuals by addressing underlying risk factors that increase the likelihood
that an individual will become a victim or perpetrator of violence. By definition,
public health aims to provide the maximum benefit for the largest number of
people. Programs for primary prevention of violence based on the public
health approach are designed to expose a broad segment of a population to
prevention measures and to reduce and prevent violence at a population level.’
Public health approaches can be identified by
the following characteristics:
• defining and monitoring the
problem
• identifying causes of the
problem, the factors that increase or decrease the risk of violence, and the
factors that could be modified through interventions
• designing, implementing, and
evaluating interventions to find out what works
• implementing effective and
promising interventions on a wider scale, while continuing to monitor their
effects, impact, and cost-effectiveness (WHO, 2017a).
According
to Anikweze( 1998), the
perspective of public health on the Violence
Prevention Alliance revolves around three theoretical models: the typology of
violence, the public health approach, and the ecological framework. These models
guide understanding, research, and action for violence prevention. The typology
is a tool to help organize thinking about the types of violence and how violence occurs. The public health approach offers practitioners, policymakers, and researchers a stepwise guide that can be applied to planning
programs, policies, and investigations. Finally, the ecological framework
bridges these two models, giving a structure to understanding the contexts
within which violence occurs and the interactions between risk factors in each
of these contexts and between them. The ecological framework shows where and
how to apply the public health approach and is useful for categorizing planned
or existing interventions to help understand the mechanisms by which they might
be working, John et al (2001).
2.1
Public health approach to violence?
Public health approaches work
by providing a framework that seeks to understand what causes violence and
respond with interventions to prevent or reduce violence, at the population
level, informed by the best available evidence. Public health approaches
undertake robust research and analysis to identify risk and protective factors
that are associated with violence. Definitions of risk and protective factors
are presented below.
• Risk factors are those which can usefully predict an increased likelihood of violence.
For example, communities with high levels of unemployment may be at higher risk
of experiencing increased levels of violence.
• Protective factors are factors that reduce the likelihood of violence. For example,
communities with low levels of unemployment may be at less risk of experiencing
high levels of violence.
2.2 Effectiveness of public
health approaches in reducing violence?
The public health approach
outlined above provides a useful framework for taking an evidenced-led
approach to violence reduction. As well as approaches to generating evidence
concerning the causes of violence in populations, a public health approach can
also deploy a range of interventions aimed at reducing violence at the
population level (CDC,2006).
2.3 Interventions aimed at
supporting parents and families
• The Family Nurse Partnership
• Incredible Years of Preschool
• Family Foundations
• Triple P
• Empowering Parents
Empowering Communities
Developing life
skills in children and young people
• The Good Behaviour Game
• Incredible Years Child
Training (Dinosaur School)
• Incredible Years of Teacher
Classroom Management
• Promoting Alternative
Thinking Strategies (PATHS)
• Let’s Play in Tandem
Working with high-risk
youth and gangs/community interventions
• Community Initiative to
Reduce Violence (CIRV)
Identification, care, and
support
• Identification and referral
to improve safety (IRIS)
Multi-component
interventions
• Multisystemic therapy Obi
(2007).
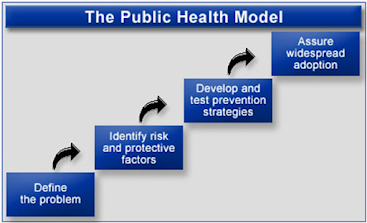
2.3 Steps of the public health approach
Adapted from CDC
(2015)
When considering public health
approaches and the implementation of interventions to reduce violence, we
consider the following:
1. Surveillance. What is
the problem?
• Define the issue. This includes conducting a robust needs assessment concerning violence,
including types of violence as well as gaining a clear understanding of risk
and protective factors that can be targeted in individuals, families,
communities, and populations to address and reduce violence at a population
level.
2. Identify risk and protective
factors. What are the causes?
• Understand the causes of violence.
This includes taking an
evidence-led approach to understanding which risk and/or protective factors
cause the violence issue and how they interplay. Through achieving this understanding,
local areas are more likely to be successful in implementing public health
interventions that effectively moderate and address risk factors and strengthen
protective factors, ultimately reducing violence at a population level.
3. Develop and identify
interventions. What works for whom?
• Develop an anti-violence or reducing violence strategy. Critically, this strategy should respond to an identified need in the population under consideration and focus on addressing
the causes of violence. The strategy should be developed and agreed upon between
stakeholders and be Specific, Measurable, Achievable, Relevant, and Timebound.
The strategy should link to the wider strategic and policy context and include
collaborative and co-productive development with local partners, including the
local community, which should ensure local ownership of the strategy and help
to ensure that it is implemented as intended.
• Commission and fund evidence-based interventions that
have been shown to reduce violence. Where possible, local areas should consider commissioning and funding
evidence-based interventions that have been shown to reduce violence.
• Don’t be afraid to innovate.
If there are no off-the-shelf’
evidence-based interventions available, then interventions should be developed
based on existing evidence for what works in modifying risk and
protective factors for the particular kinds of violence problem that the area
is aiming to address.
4. Implementation. Scaling
up effective programs and interventions
• Implement interventions ensuring that fidelity is maintained in line with what has been demonstrated to work.
Model fidelity means ensuring
that the model implemented stays loyal and is delivered as close to the
original model as possible. This requires careful consideration when taking
into account the context into which the intervention is being rolled out. Not
ensuring model fidelity is one of the key reasons why the implementation of
interventions that have been evidenced to work in one area do not work in
another.
• The implementation of interventions takes time to embed
in practice and to achieve outcomes.
Local decision-makers need to
provide sufficient time for programs and interventions to impact desired
outcomes. It can sometimes take over five years for programs to achieve
outcomes.
• Evaluate and monitor the success of public health
interventions.
This review shows that there
is still work to be done in developing and evaluating public health
interventions aimed at reducing violence at a population level. Although
resources are often tight, you should aim to contribute to the evidence base by
ensuring robust evaluation of public health interventions that are commissioned
and funded. Robust evaluation can save money by clearly identifying models and
practices that work, but also showing what does not work. Knowing this can save
money and use scarce resources more effectively in the long term.
Public health interventions
operate by modifying the risk factors that make an individual, family, or
community vulnerable to violence (as victims, perpetrators, or both) and by
promoting protective factors.
2.4 The ecological framework
The ecological
framework is based on evidence that no single factor can explain why some
people or groups are at higher risk of interpersonal violence, while others are
more protected from it. This framework views interpersonal violence as the
outcome of interaction among many factors at four levels—the individual, the
relationship, the community, and the societal.
- At
the individual level, personal history and
biological factors influence how individuals behave and increase their
likelihood of becoming a victim or a perpetrator of violence. Among these
factors are being a victim of child maltreatment, psychological or
personality disorders, alcohol and/or substance abuse, and a history of
behaving aggressively or having experienced abuse.
- Personal relationships such
as family, friends, intimate partners, and peers may influence the risks of
becoming a victim or perpetrator of violence. For example, having violent
friends may influence whether a young person engages in or becomes a
victim of violence.
- Community contexts in which social relationships occur, such as
schools, neighborhoods, and workplaces, also influence violence. Risk
factors here may include the level of unemployment, population density,
mobility, and the existence of a local drug or gun trade.
- Societal factors influence whether violence is encouraged or
inhibited. These include economic and social policies that maintain
socioeconomic inequalities between people, the availability of weapons, social and cultural norms such as those around male dominance over
women, parental dominance over children, and cultural norms that endorse
violence as an acceptable method to resolve conflicts.
The ecological
framework treats the interaction between factors at different levels with
equal importance to the influence of factors within a single level. For
example, longitudinal studies suggest that complications associated with
pregnancy and delivery, perhaps because they lead to neurological damage and
psychological or personality disorder, seem to predict violence in youth and
young adulthood mainly when they occur in combination with other problems
within the family, such as poor parenting practices. The ecological framework
helps explain the result—violence later in life—as the interaction of an individual
risk factor, the consequences of complications during birth, and a related risk factor, the experience of poor parenting. This framework is also useful to
identify and cluster intervention strategies based on the ecological level in
which they act. For example, home visitation interventions act at the
relationship level to strengthen the bond between parent and child by
supporting positive parenting practices.

The ecological framework:
examples of risk factors at each level
Adapted from WHO
(2017b)
2.5 Types of
public health interventions for violence prevention/reduction
Central to an effective public
health approach to reducing violence is the implementation of interventions
that successfully address risk and protective factors in individuals, families,
communities, and populations to reduce violence at a community and/or population
level.
However, definitions varied
and there was no clear consensus or definition as to what constitutes a public
health intervention to reduce violence, apart from that it should reduce
violence at the community and/or population level.
Conaglen and Gallimore (2014)
describe violence prevention interventions as operating on various levels
(primary, secondary or tertiary) and define interventions to address violence
as universal, selected, or indicated.
2.6 Levels of violence prevention
Adapted from WHO
(2019)
Primary – preventing violence before it happens, i.e., reducing the number of new cases of violence in the population.
Secondary – immediate responses to incidents of violence to
decrease prevalence after early signs of the problem, i.e. to reduce the
prevalence of violence in the population.
Tertiary – to intervene once the violence problem is
evident and causing harm.
Types of
intervention to address violence
Universal – aimed at a general population
Targeted
selected – targeted at those more at
risk
Targeted
indicated – targeted at those who use
violence
While the WHO, Bellis et al.
(2012) and others provide clear definitions of public health approaches, there
is less clarity in the literature about what kinds of interventions fall within
the scope of a public health approach. This is complicated by the fact that the
position of an intervention in the matrix (i.e., primary, secondary, tertiary,
universal, targeted selected, targeted indicated) is rarely explicit. However,
public health interventions, like public health approaches should seek to
reduce violence at a community and/or population level.
3.0 CONCLUSION
The preceding discussions have shown that violence is an ill wind of
social phenomenon, which blows no one any good. In its aftermath both its
perpetrators and victims are losers. As a way out of the mess, Nigerian policymakers should imbibe the public health
approach while working on violence prevention and reduction in the country.
References
AfrolNews (2007) Half
of Nigeria’s Women experience domestic violence. retrieved May 22, 2008,, from
http://www.afro.com/ articles/16471
Anikweze C. M. (1998)
Threats to adolescent well being. In Orji S.A and C. M. Anikweze (eds.)
Adolescent Psychology. 109 – 117.
BBC News Education (2003) Violence at Home
hits children’s IQ. Retrieved May 2008 from http://news.bbc.co.uk/1/hi/
education/2981312.stm.
Catalano, R; Lind, S, Rosenblatt, A and R
Novaco (2003) Research into the Economic antecedents of Violence. American
Journal of Community psychology.
CDC (2006) Intimate Partner Violence – fact
sheet. Retrieved Oct. 2008
Dahlberg, L. L. and E. G Krug (2002) Violence
– a global public health problem. In King E, Dahlbergl, Meray J. A and A. B
Zwi, Lozano R (eds.)
World Report on violence and health. Geneva.
Switzerland: WHO, 1-56. Dobson (1984) Dare to Discipline. Weston Illinois:
Tyndale House Publishing
Obi, S. N., and B.C.
Ozumba (2007) Factors associated with domestic violence in South-East Nigeria.
Journal of obstetrics and gynecology. 27. (1) 75 – 78. Prevalence of Domestic
Violence in Nigeria: Implications for Counselling
Richie, O. N. 8 Straus, M. (1994) Beating the
devil out of them; Corporal Punishment in American families. New York.
Lexington Books
UNICEF (2001) Children
and Women’s rights in Nigeria: A wake-up call situation assessment and
analysis. Edited by Hodge. Abuja: National Population Commission and UNICEF.
UNICEF (2005) Violence at home (archive)
Voices of Youth Forum. Retrieved Oct. 2008
Dahlberg
LL, Krug EG. Violence: a global public health problem. In: Krug E, Dahlberg LL,
Mercy JA, Zwi AB, Lozano R, eds.
World Report on Violence and Health.
Geneva, Switzerland: World Health Organization; 2002:1-21.